What is prostatic artery embolization (PAE)?
- Francesco Bruno Tagliaferro
- Jul 22, 2023
- 7 min read
Updated: Jul 23, 2023
Prostatic artery embolization (PAE) is a minimally invasive procedure for the treatment of benign prostatic hypertrophy (BPH). PAE is performed under local anesthesia by Interventional Radiologists.
PAE is based on the endovascular occlusion (embolization) of the arteries that carry blood to the prostate. This procedure induces the controlled ischemia of a portion of the prostate and the subsequent and progressive reduction of the prostate volume and therefore of the urinary symptoms.
BENIGN PROSTATIC HYPERTROPHY (BPH)

The prostate is a gland of the male reproductive system located between the bladder and the rectum. It extends all the way around the initial part of the urethra, which is therefore located in the prostate (prostatic urethra).
The main role of the prostate is to produce seminal fluid, one of the components of sperm, with the task of nourishing and transporting sperm.
Benign prostatic hypertrophy (BPH) is a non-cancerous, benign, enlargement of the prostate. It is an extremely common condition: it affects about 50% of men in their 50s and over 90% of men over the age of 80.
SYMPTOMS
The symptoms of BPH are caused by the compression exerted by the gland on the urethra. These are:
Urinary hesitancy (difficulty in starting urination)
Intermittent urinary flow
Feeling that the bladder has not completely emptied after urinating
Weak urine flow
Increased frequency of urination (pollakiuria), also at night (nocturia)
Urgency (a need to empty the bladder that cannot be delayed)
Dysuria: painful urination
Incontinence
Importantly, prostate size does not necessarily correlate with symptom intensity: even relatively small prostates can cause significant symptoms. The symptoms' intensity is in fact determined by the sum of two factors:
the static obstruction, related to prostate size. The larger the prostate, the greater the compression on the prostatic urethra.
the dynamic obstruction, due to the compression exerted on the prostatic urethra by the smooth muscle of the bladder neck, the prostate and its capsule.
The severity of the symptoms (mild, moderate or severe) is assessed using the IPSS questionnaire, which is also a useful aid in verifying the effectiveness of therapeutic interventions.
DIAGNOSIS
Rectal exploration may reveal a prostate enlargement.
PSA is evaluated with a blood draw. It is non-specific: if elevated it can indicate both benign conditions (infections, BPH, trauma, etc.) and malignant pathologies (carcinoma).
A PSA increase requires careful monitoring and more in-depth examinations.
Uroflowmetry is a very useful, non-invasive test, which allows to evaluate and objectify the urinary flow. It is also a valuable tool for monitoring the results of a treatment.
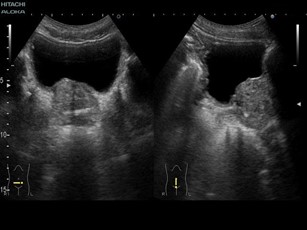
The suprapubic prostate ultrasound is a simple examination that evaluates the prostatic diameters and estimates the size of the gland. At the same time, the bladder is studied, evaluating, in particular, the thickness of the wall, the presence of any diverticula, and the quantity of residual urine after urination.
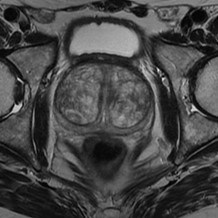
Multiparametric prostate MRI, with contrast medium, is crucial in the preparation of a prostate embolization procedure, due to the wealth of information it provides regarding the anatomy of the prostate (both general and zonal prostate volume, dimensions of the middle lobe and possible protrusion into the bladder, characterization of the peripheral and central area of the gland, vascularization), for the detection of areas suspicious for neoplasia that would contraindicate the procedure), for the possibility of studying the entire pelvic compartment (pelvic lymph nodes i, bladder anatomy, etc.) with a panoramic view not allowed by the ultrasound.
The Angio-RM study allows evaluating the pelvic arterial vessels for precise preoperative planning.

Fusion-guided prostate biopsy. Prostate cancer must be excluded before the embolization. Magnetic resonance allows you to identify suspicious prostatic areas which, if present, must be subjected to fusion-guided prostate biopsy (i.e. an ultrasound-guided biopsy that superimposes the images of the multiparametric MRI of the prostate on those of the trans-rectal ultrasound that is performed during the biopsy).
THE TREATMENT OF BENIGN PROSTATIC HYPERTROPHY
Treatment is usually initially pharmacological. In case of failure, surgery or interventional radiology (prostate artery embolization) may be necessary.
Drug therapy
Alpha blockers (doxazosin, terazosin, alfuzosin, tamsulosin): relax the muscles of the prostate and bladder neck and increase the urinary flow rate.
5α-reductase inhibitors (finasteride, dutasteride). In association with alpha blockers, determine the reduction of the prostate s0ize.
Surgical treatments
Transvesical (ATV) or infravesical (Millin) open surgery adenomectomy. The prostate adenoma is removed through a traditional surgical cut. Still practiced in case of very voluminous prostates. It is burdened by high postoperative morbidity.
Transurethral resection of prostate adenoma (TURP). The resection of prt of the prostate through the urethra. It doesn't need surgical cuts and allows for a faster post-operative recovery.
New methods, including transurethral vaporization of the prostate (DVT), TURP laser, visual laser ablation (VLAP), Transurethral Microwave Thermo Therapy (TUMT), Transurethral needle ablation of the prostate (TUNA).
PROSTATIC ARTERY EMBOLIZATION (PAE)
Prostatic artery embolization is a minimally invasive procedure for the treatment of benign prostatic hypertrophy. It consists in the selective embolization (occlusion) of the prostatic arteries, thus causing a therapeutic ischemia of part of the gland.
WHEN IS IT INDICATED?
It is indicated in case of symptomatic prostatic hypertrophy (moderate/severe symptoms) in patients (one or more of the following)
for whom drug treatment is ineffective or not tolerated
with high surgical risk
who prefer a minimally invasive procedure
WHEN IS IT CONTRAINDICATED
Prostate cancer
Urethral strictures
Kidney failure
Stones in the urinary tract with surgical indication
Urinary tract infections
Previous severe allergy to organo-iodinated contrast medium
BEFORE THE INTERVENTION
Before the procedure, the clinical evaluation by the interventional radiologist is necessary to assess the effective indication for the procedure and the absence of contraindications. The interventional radiologist will also expose to the patient the pros and cons of the various techniques currently available.
Prostate cancer must be ruled out. Therefore, it is essential to perform a multiparametric MRI of the prostate before surgery, and possibly, if this is positive, a fusion guided prostate biopsy.
Blood samples are necessary, including at least a complete blood count, coagulation status and renal function.
The patient needs to fast at least 12 hours.
A bladder catheter is inserted before the procedure and remains in place for the duration of the procedure.
HOW IS PAE PERFORMED?
Prostatic artery embolization is a minimally invasive procedure performed under local anesthesia.
In the angiography operating room, in a strictly sterile environment, the patient is placed in a supine position on the operating table and is prepared as for any other operation (hair removal, skin disinfection, preparation of the operating field, etc.).
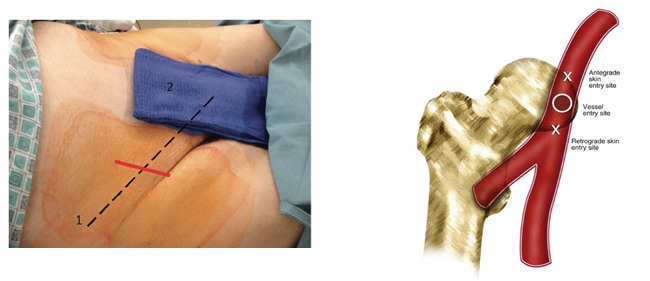
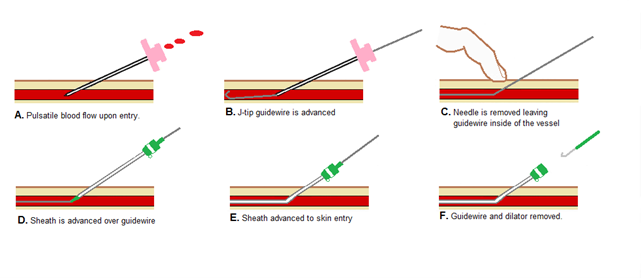
The Interventional Radiologist, after performing local anesthesia, performs an ultrasound-guided arterial puncture of the common femoral artery (right or left or both), at groin level, and inserts a vascular introducer, a plastic cannula with a diameter of a few millimeters equipped with an anti-reflux valve that allows you to work in the artery without blood leakage.
After inserting the vascular introducer, without further cuts, the Interventional Radiologist (IR), guided by the X-rays images, navigates inside the patient's arteries through small catheters (plastic tubes of various shapes) and positions a microcatheter (with a even smaller diameter) in the arteries that vascularize the prostate; here the IR releases micro-particles in a super-selective way occluding the target vessels.


The aim is to induce a controlled ischemia of part of the prostate, which has a double effect: reduction of the prostate size, and therefore reduction of the static obstruciton; prostatic "relaxation", the relaxation of the smooth muscle cells of the bladder neck, prostate and prostatic urethra, with reduction of the dynamic component of the symptoms.
After the procedure, the arterial catheters are removed and the arterial access is closed, with dedicated devices and manual compression, without the need to apply any stitches, as no surgical incisions have been made.
AFTER THE PROCEDURE
Once the procedure is finished, the patient returns to the ward. The bladder catheter is kept in place for the duration of hospitalization, during which the patient will have to lie in bed and move as little as possible to avoid bleeding from the arterial access.
In patients with chronic bladder catheters, a first attempt to remove them is made after one week; if there isn't spontaneous urination, the catheter is positioned again and a new attempt is repeated after another seven days, and so on until the result is obtained.
The discharge takes place within 24 hours of the procedure.
The Interventional Radiologist will prescribe an antibiotics and corticosteroids therapy for 5-7 days and an anti-inflammatory therapy to be taken as needed. Any problem relating to the pathology or to the intervention must be referred to the Interventional Radiologist who performed the procedure or to the referring Urologist.
RESULTS
The first results are generally immediate, but sometimes it takes time for the embolization to exert its full effects, with a progressive improvement of the symptoms that goes on for a few days or weeks, until the full effectiveness of the ischemia is reached.
Numerically, the results are as follows.
Technical success (intended as the success of the procedure): 75-94.3%
Reduction of symptoms
3 months: 80.7-97.1%
12 months: 75.2%
24/36 months: 72%
Bladder catheter removal in patients with indwelling catheters: 91-100%
Prostate volume reduction: 20-40%
It is noteworthy that in almost all patients with indwelling bladder catheters, who cannot urinate spontaneously, the effectiveness of embolization in removing the catheter is very high, over 90%.
Another thing to note is that the reduction in prostate volume does not correlate proportionally with the reduction in symptoms. In fact, the volume may decrease by a little, but the symptoms by a lot, and this apparent discrepancy is determined by the action on the dynamic component of the prostatic obstruction.
The reduction of prostate size, in itself, is not the goal of the intervention, and in hindsight it is not even the reason why patients go to the doctor. It is the symptoms, brought about by the BPH, that are a problem, and these are treated.
COMPLICATIONS
During the first 3-5 days, it is not uncommon for dysuria (painful sensation when urinating) and increased frequency of urination to occur, but these symptoms are mild and self-limiting.
Quite common is the so-called Post-Embolization Syndrome, characterized by the onset, a few days after the procedure, of prostatic burning, moderate pelvic pain, small amounts of blood in the urine and/or faeces mixed with mucus, all lasting 2-3 days; non-specific systemic symptoms may also present, which include fatigue, loss of appetite, malaise, low-grade fever. These symptoms are easily manageable with adequate medical therapy with anti-inflammatories.
The major complications specific to the operation (in addition to those generic to endovascular procedures) are determined by non-target embolization, i.e. ischemia of other organs than the prostate. This happens because some of the arteries that vascularize these other organs, such as for example the rectum and the bladder, can be in connection with the prostatic arteries and are so small in size that they are not easily detectable, and therefore a part of the embolizing material can pass unnoticed into these vessels, and cause an involuntary ischemia of other tissues.
Careful planning, and above all careful execution, of the intervention, minimize this risk.
Most of the time, in any case, this type of complication is very annoying but resolves without permanent consequences to the functionality of the affected organs.
Minor complications (17,7%)
Post-PAE syndrome: common. Prostatic burning, pelvic pain, nonspecific systemic symptoms. Small amounts of urine, rectal or seminal blood. Lasts 3-5 days. Treated with NSAIDs, analgesics and antiemetics
Urinary tract infections
Prostatitis
Arterial access site complications
Major complications (2,9%)
Non-target embolization: bladder, rectum, bone, etc.
POST-OPERATIVE FOLLOW-UP
The follow-up visit will be made one month after the operation.
After that, the advice is to perform a urological visit with uroflowmetry every 12 months to evaluate the urinary symptoms.
It is good practice to measure PSA every 12 months, regardless of the procedure.


Yorumlar